Xerosis: Symptoms, Causes and Treatment Tips
It’s like dry skin but worse--and it can leave your skin rough and cracked. It’s xerosis. In fact, untreated xerosis can put you at risk for a bacterial infection. One of the first signs of xerosis is a scaly pattern of dry skin on your arms or legs. By figuring out what is causing your abnormally dry skin and by adding intense moisturizers to your skincare routine, you can heal xerosis and bring your skin back to life.

What is Xerosis?
Xerosis cutis (pronounced zi-roh-sis kyoo-tis) is the medical term for abnormally dry skin. A less severe form of xerosis is xeroderma or normal dry skin. While xerosis is often a temporary condition that leaves the skin looking scaly, it can also cause discomfort, itchiness, and inflammation. If left untreated, this condition can cause breaks or cracks in the skin and lead to bacterial infection.
Signs of Xerosis
If your skin feels tight, uncomfortable, or itchy, you may be suffering from xerosis. Common symptoms of xerosis include:
If your symptoms are more severe than the telltale signs of xerosis, you may have severely dry skin.
Xerosis Causes
Xerosis is caused by lack of moisture in the skin, which may be the result of aging or an underlying condition or disease. The elderly and those with diabetes have a higher risk of developing xerosis cutis. Dr. Simone McKitty, Board-Certified Dermatologist at McKitty Dermatology, tells us that “skin conditions such as atopic dermatitis, keratosis pilaris, ichthyosis, and psoriasis also cause dry skin and if left untreated, these conditions can worsen and lead to bleeding and cracking.” Additional causes of xerosis may include:
If left untreated, xerosis can lead to more severe skin conditions like a fungal or bacterial infection. Red, sore patches on your skin may be an early sign of infection.
Treatments for Xerosis
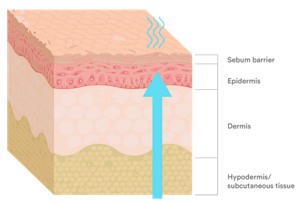
Xerosis is often painful, irritating, and can damage your skin in the long run. Treating xerosis is vital for keeping your skin healthy and increasing its ability to protect you from infection and disease. Treating xerosis is similar to how you get rid of dry skin and is possible with the help of the right products and skincare routine. Your skin is your largest organ so let’s learn some tips for keeping it healthy and xerosis-free!
1. Eliminate Ingredients That Dry Out Skin
The first thing you should do to combat xerosis is to take a look at your current products. If any of your existing products contain the ingredients sodium lauryl sulfate, triclosan, lye, alcohol, retinoid, and alpha-hydroxy acid or added fragrance, they might be contributing to your dry skin.

2. Try Natural Solutions for Dry Skin
“Sunflower seed oil and coconut oil are two natural ways to improve hydration when they are used as a moisturizer,” says Dr. McKitty. “Oatmeal is another natural ingredient that can be used to help treat dry skin. Adding powdered oatmeal to a bath or using creams that contain oatmeal may help to relieve moderately dry skin.” Applying honey to your skin is also a great natural option for dry skin. A recent study found that honey is one of the most effective natural moisturizers, so it is an excellent solution for dry, itchy skin.
3. Moisturize Daily
For ultimate skin hydration be sure to apply moisturizer immediately after every shower, when your skin is clean and your pores are open. A great option for after-shower hydration is to use an in shower lotion. For severe cases of xerosis, apply an ultra healing lotion or cream in the evening before bed to help accelerate skin’s healing.. Once the condition of the skin improves you should be able to go down to one application of a moisturizer a day. Dr. McKitty told us that “The best way to prevent xerosis is with regular use of a good therapeutic moisturizer that contains a humectant such as glycerin or urea.”
4. Use a Gentle Cleanser
Avoid harsh, alcohol-based cleansers that remove your skin’s natural oils. Instead, look for mild, fragrance-free cleansers containing propylene and glycerin.
5. Exfoliate Gently
Exfoliating with a wet towel or exfoliating cleanser can help remove dry skin flakes and refresh your skin. Dr. McKitty explains that “Light exfoliating is okay to help remove dry skin flakes, but be careful to not be too excessive with exfoliating as it can overstrip and damage your skin.” After exfoliating, apply an intensive moisturizer to your skin to prevent moisture loss.
6. Take Cooler Showers
Hot water strips away your skin’s natural moisture barrier, which can worsen symptoms of xerosis. Cold or lukewarm showers, while not as soothing as hot showers, are much gentler on the skin. If you’re suffering from skin conditions like xerosis, eczema, or psoriasis, cooler showers can help your skin retain moisture as it heals.
7. Take Shorter Showers
In addition to shower temperature, the length of your shower can also impact your skin’s condition. The longer you stay in the shower, the more natural oils are removed from your skin. Keep showers between 5 to 10 minutes; any longer and your skin will likely be less hydrated than when you started.
8. Eat a Healthy Diet
It’s important to eat a well-balanced diet to maintain your overall health, and loading your plate with Omega 3-fatty acids will help keep your skin hydrated. Omega 3-fatty acids help to build up your skin’s natural moisture barrier and are present in foods like fish and flax seeds. Adding vitamins C, D, E and K and well as zinc and copper can help keep your body hydrated and protect it from dryness.
9. Stay Hydrated
Water helps moisturize the skin by hydrating the cells inside your body and flushing out toxins that may be contributing to dry skin. According to the USGS , an adult male should drink about 3 liters of water throughout a day and an adult female should drink about 2.2 liters. To get even more hydration during the day, add foods with high water content such as watermelon, celery, and cucumbers to your diet.
10. Add Moisture to the Air
Living in low-humidity climate or using centralized heat sources in winter months, can suck moisture out of your skin. Keep your skin feeling soft and smooth by using a humidifier regularly. Warm mist humidifiers work to supplement moisture in the air and stop the moisture in your skin from evaporating.
11. Protect Your Skin from Winter Weather
Although we’re usually bundled up during winter months, sometimes we leave our hands, face, and neck exposed. When you’re outside, wearing a scarf and gloves can help prevent chapped lips as well as xerosis on your face and hands.
12. Limit Sun Exposure
On the opposite end of the spectrum, sun exposure can also contribute to xerosis symptoms. While the sun is a terrific natural resource of vitamin D, it also decreases the amount of moisture and oils in the surface of the skin. The Skin Cancer Foundation recommends wearing a broad spectrum sunscreen with at least SPF 30 whenever outdoors. (2)
13. Ask About Prescription Medication
If you have tried all the tips above and are still experiencing extreme dryness, talk with your dermatologist about prescription medicines. To reduce itching and irritation caused by xerosis, your dermatologist may recommend a topical steroid medication, like 1 percent hydrocortisone cream.
When to See a Dermatologist
If you have persistent skin irritation and over-the-counter medications aren’t helping, we recommend visiting a dermatologist as soon as possible. Seek immediate medical care from a dermatologist if you notice any of these symptoms:
“If you have xerosis that doesn't get better within two weeks, call your doctor or dermatologist,” recommends Dr. McKitty. “However, if it’s accompanied by redness, interfering with sleep, accompanied by open sores from scratching or covering a large body surface area, see your doctor or dermatologist immediately.”
Key Takeaways



